1801006078 - Long Case
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centred online learning portfolio and your valuable comments on comment box is welcome. I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CASE
This is a case of a 50 year old male, a resident of Miryalguda, factory worker by occupation, presented with the chief complaints of -
Weakness of right upper and lower limbs with slurring of speech and deviation of mouth to the left since 5 days
HISTORY OF PRESENTING ILLNESS:-
1 month ago he developed giddiness and weakness of left upper and left lower limb which was sudden in onset followed by fall. He was then taken to the hospital where he was treated for the same and diagnosed with hypertension. His symptoms resolved in around 3 days. The patient was compliant with his hypertension medication for 20 days and stopped taking it after that.
The patient then developed weakness of right upper limb and lower limb 3 days ago which was sudden in onset. He noticed the weakness on his right side when he woke up in the morning. He felt unsteady as he stood up after waking up.
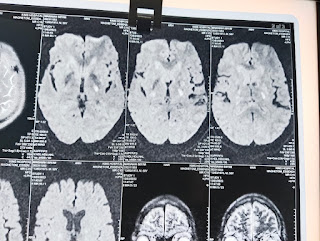
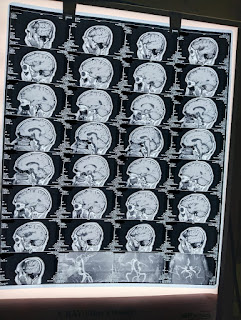
The weakness of right side was also associated with slurring of speech and deviation of the mouth to his left side. He was taken to a hospital nearby where he underwent a CT scan. He was then referred to our hospital the next day.
There is no history of difficulty in swallowing, behavioural abnormalities, fainting, sensory disturbances, fever, neck stiffness, altered sensorium, headache, vomiting, seizures, abnormal movements, falls.
PAST HISTORY:-
The patient was apparently asymptomatic 30 years ago. He then sustained a fracture close to his right elbow. He currently cannot extended his elbow completely.
He is known case of hypertension from past 1 month
No history of diabetes, asthma, TB, epilepsy, coronary artery disease, or any thyroid abnormalities.
PERSONAL HISTORY:-
( daily routine )
The patient wakes up at 4:00am in the morning daily. He has tea and goes to work in the ice factory. He lives very close to the ice factory. He comes home and has breakfast at around 8 to 9 am. He usually has rice and curry for breakfast. He then goes back to work and comes home for lunch at around 2:00 pm. He usually has rice with curry and dal for lunch. He consumes chicken or mutton thrice weekly. He sometimes takes a nap in the afternoon depending on his work for the day. He finishes work by around 6:00 pm following which he comes home, has tea and takes a bath. Sometimes he works until 9:00 pm. He sleeps by 9:00 pm.
The patient has been chewing tobacco for around 10 years. 1 packet of tobacco lasts for 2 days.
He consumes alcohol on a regular basis since 30 years. He stopped for around 3 years and started again 6 months ago after the death of his daughter’s husband.
Bowel and bladder movements are regular.
TREATMENT HISTORY:-
He consumed medication for hypertension - Amlodipine and Atenolol for 20 days which he stopped around 10 days ago.
FAMILY HISTORY:-
No similar complaints in the family.
GENERAL EXAMINATION:-
Patient is conscious, cooperative, with slurred speech
Well oriented to time, place and person
Moderately built and moderately nourished.
Vitals :-
Temp - afebrile
BP - 140/80 mm Hg
Pulse rate - 78 bpm
Respiratory rate - 14 cycles per minute
Pallor - absent
Icterus - absent
Cyanosis - absent
Clubbing - absent
Lymphadenopathy - absent
Oedema - absent
SYSTEMATIC EXAMINATION:-
1) CNS EXAMINATION :-
Higher mental functions are intact
No meningeal signs
Glasgow scale - 15/15
Gait - walks only with support
Cranial nerves -
I - no alteration in smell
II - no visual disturbances
III, IV, VI - eyes move in all directions
V - sensations of face normal, can chew food normally
VII - Deviation of mouth to the left side, upper half of right side and left side normal
VIII - hearing is normal, no vertigo or nystagmus
IX,X - no difficulty in swallowing
XI - neck can move in all directions
XII - tongue movements normal, no deviation
Pupils - both are normal in size, reactive to light
Motor Pathway:-
Power:-
Rt UL - 3/5 Lt UL-5/5
Rt LL - 3/5 Lt LL-5/5
Tone:-
Rt UL - Increased
Lt UL- Normal
Rt LL- Increased
Lt LL- Normal
Reflexes:
Right Left
Biceps.
+++ ++
Triceps.
+++ ++
Supinator.
+++ ++
Knee.
+++ ++
Ankle.
+++ ++
Plantar:
Muted Flexion
Involuntary movements - absent
Fasciculations - absent
Sensory system -
Pain, temperature, crude touch, pressure sensations normal
Fine touch, vibration, proprioception normal
No abnormal sensory symptoms
Cerebellum -
Finger nose test normal, no dysdiadochokinesia, Rhomberg test could not be done
Autonomic nervous system - normal
Examination Videos:- Link for videos
2) CVS EXAMINATION :-
JVP: Normal
INSPECTION:
Chest wall symmetrical
Pulsations not seen
PALPATION:
Apical impulse – normal
Pulsations – normal
Thrills absent
PERCUSSION:
No abnormal findings
AUSCULTATION:
S1, S2 heard
No murmurs
No added sounds
3) ABDOMINAL EXAMINATION :-
INSPECTION:
1. Shape – flat
2. Flanks – free
3. Umbilicus – Position-central, Shape-normal
4. Skin – normal
5. Hernial Orifices - normal
PALPATION:
Abdomen is soft and non tender
No hepatomegaly
No splenomegaly
Kidneys not enlarged, no renal angle tenderness
No other palpable swellings
Hernial orifices normal
PERCUSSION:
Fluid Thrill/Shifting dullness/Puddle’s sign absent
AUSCULTATION:
Bowel sounds – normal
No bruits, rub or venous hum
4) RESPIRATORY EXAMINATION :-
- Chest bilaterally symmetrical, all quadrants
moves equally with respiration.
- Trachea central, chest expansion normal.
- Resonant on percussion
- Bilateral equal air entry, no added sounds heard.
1. Breath sounds - Normal Vesicular Breath sounds
2. Added sounds - absent
3. Vocal Resonance - normal




















Comments
Post a Comment